Abstract
Introduction:
Persons with hemophilia (PWH) who develop need for surgery usually require a huge amount of clotting factor concentrate (CFC) infusion to manage their bleeding during the procedure and up to a few days or weeks afterwards until they achieve tissue healing. Managing such patients in a resource limited setting (RLS) is challenging endeavor due to limited availability of clotting factor concentrates to replace their specific deficient clotting factor. The peri-operative treatment for PWH who have antibodies against CFC is even more complicated because by-passing agents (BPA) remain largely unavailable and require more frequent administration. Health care institutions in most RLS depend on limited donations of these products and therefore surgical procedures performed require intricate planning to enable the use of the minimum required CFC or BPA to achieve optimal hemostasis. We sought to highlight our experience in managing patients with Hemophilia A who have antibodies against CFC who presented with need for surgery at Moi Teaching and Referral Hospital in western Kenya.
Methods:
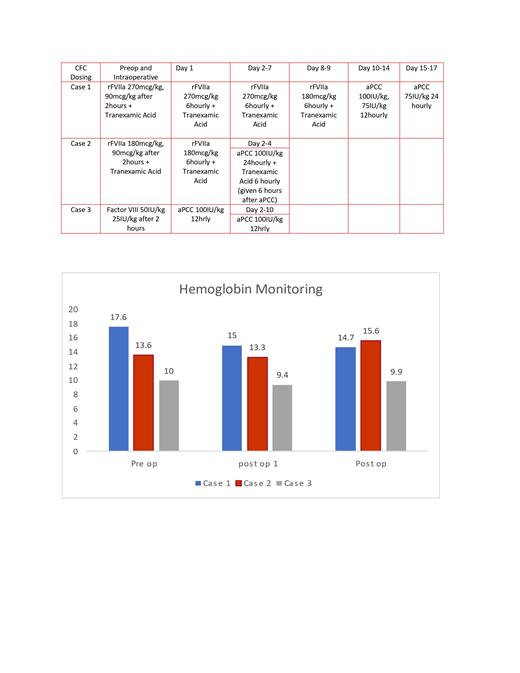
We reviewed patients charts of PWH A who presented at MTRH for surgery between 2020 and 2021 and documented their factor levels, blood counts and inhibitor levels. Three PWH A had high responding inhibitor levels. The clotting factor concentrates (CFC) used were a combination of activated Prothrombin Complex Concentrates (aPCC) and recombinant Activated Factor VII (rFVIIa) with Antifibrinolytics to achieve hemostasis. Hemostasis was monitored by the patients' hemoglobin levels (Hb) in grams per deciliter (g/dl), clinical examinations of the surgical sites and patients reported symptoms.
Results:
Case 1: 42-year-old with severe hemophilia A and inhibitor of 143BU, presented with femur fracture needed fixation with platting. Surgery was done one year after the injury because of unavailability of adequate bypassing agents during the time of injury. Day 1-7 of surgery, patient was given rFVIIa 270mcg/kg 6hourly with Tranexamic acid, then reduced at 180mcg/kg 6hourly on days 8-9 post surgery. He was then switched to aPCC 100IU/kg first dose then at 75IU/kg 12hourly on days 10-14, then at 75IU/kg 24hourly days 15-17. Tranexamic acid was stopped before infusion of aPCC. Just after the surgery, was transfused two units of blood. He was started physiotherapy day 14 post-operation. Patient pre-operative Hb was at 17.6g/dl, the Hb post-operation remained stable between 15g/dl and 12g/dl. There was some blood oozing noted during the first change of dressing but site remained clean and dry with reduction of limb swellings by 3cm.
Case 2 : 8-year-old with severe hemophilia A and inhibitor of 6BU, had bilateral undescended testis needed bilateral orchidopexy and circumcision. The surgery proceeded after 2 months of the schedule. He was given rFVIIa at 180mcg/kg 6hourly on Day 1 and 2 of surgery with Tranexamic Acid 8 hourly. On the evening of day 2 post surgery, he was switched to aPCC at 100IU/kg 24hourly to day 4 post surgery. He continued with Tranexamic acid 6 hourly, given 6 hours after aPCC infusions. Patients Hb remained stable at 13g/dl pre and postoperatively with no noted bleeding at the surgical sites.
Case 3: 3year old with moderate hemophilia A, presented with extensive subdural hematoma causing midline shift and loss of speech, needed emergency surgery. Burr hole was done with factor replacement then noted to have inhibitor of 6BU a days after the surgery. He was immediately given aPCC at 100IU/kg 12hourly for 10 days. His Hb remained stable at 10-9g/dl pre- and post-operatively with dry surgical site. Revaluation head Computerized tomography (CT) scan showed resolving hematoma with no midline shift.
Conclusion:
All the patient had adequate hemostasis during the surgery period with only the first case needing blood transfusion. There were no reported bleeding complications or thrombosis seen post-surgery and on follow up reviews. Despite the challenges faced it was possible to achieve adequate hemostasis needed for the surgical interventions using moderate doses of BPA, attesting to the potential that RLS are capable in managing hemophilia patients with inhibitors. We recommend further studies on the minimal dosing recommendations of BPA needed to achieve adequate hemostasis in surgical management of hemophilia patients with inhibitors in resources constrained environments.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal